By Enrique Castro-Sanchez
ISID Emerging Leader
Research Lead (joint), Centre for Health Services Research
City, University of London, UK
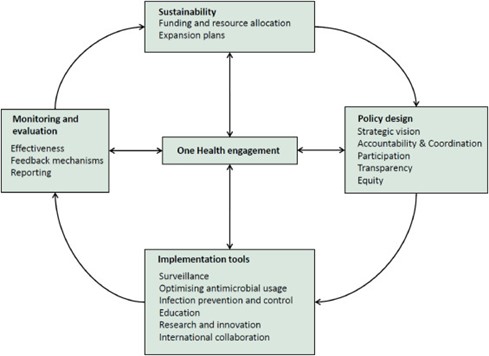
This week the World Health Assembly meets once again [https://www.who.int/about/governance/world-health-assembly/seventy-fourth-world-health-assembly] to discuss progress on the most pressing health and care issues faced by nations and citizens around the world. Unsurprisingly perhaps, the response to the SARS-CoV-2 pandemic, including continued efforts to distribute the existing vaccines effectively and equitably, takes centre stage. But many other long-standing health topics remain in the working agenda, including drug-resistant infections and the chronic shortage of health care workers worldwide.
Robust studies in hospital and primary care settings worldwide have by now undoubtedly emphasised the crucial importance of an adequate health workforce, and the benefits of satisfactory staff/patient ratios to clinical outcomes, patient safety and experience, and organisational performance [McHugh MD Aiken LH Sloane DM Windsor C Douglas C Yates P. Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: a prospective study in a panel of hospitals.
Lancet. 2021; https://doi.org/10.1016/S0140-6736(21)00768-6]. Infection prevention and control and antimicrobial stewardship programmes and have also recognised the need to increase human resources in these areas.
For example, back in 2016, the O’Neill Report [https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf] advocated for the need to engage more healthcare workers in antimicrobial stewardship interventions.