To promote education and awareness during World AMR Awareness Week, we present compelling examples that demonstrate how ISID is actively engaged in the global battle against antimicrobial resistance. Together, we can make a difference!
World AMR Awareness Week 2024 at ISID
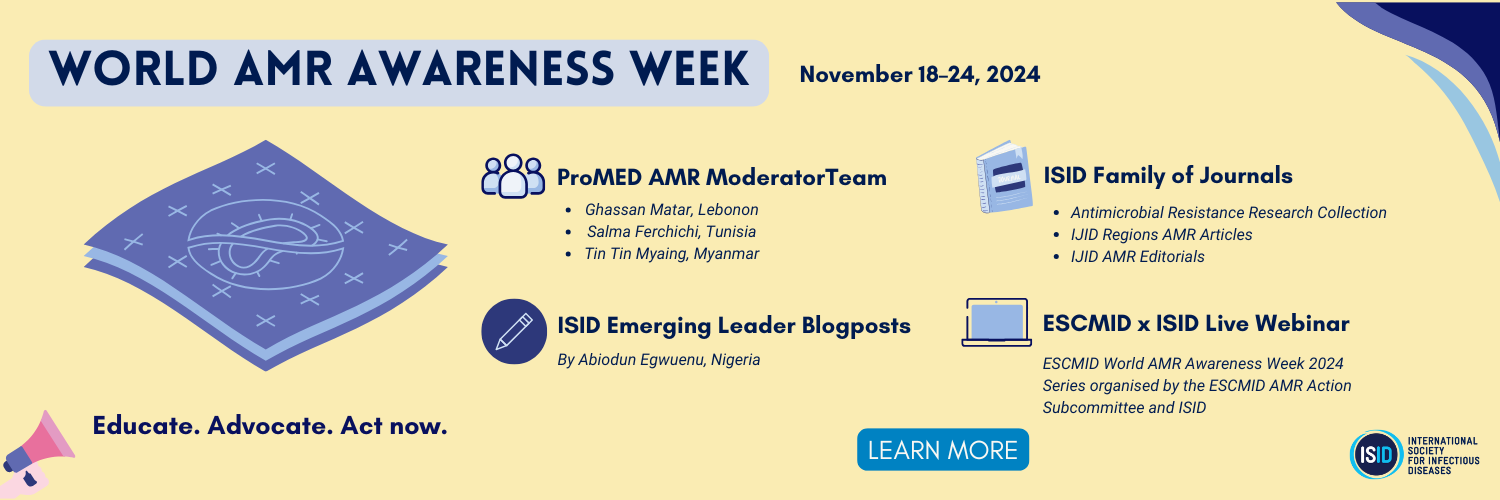
The ProMED Network & Moderator Team
ProMED has 10 different networks, with the newest one being its AMR network. This network, ProMED’s first topic-based network, was launched in 2020 and has posted over 2,000 alerts to the network to date, averaging over 650 posts per year. Over 11,000 readers subscribe to receive email updates from ProMED-AMR.
ProMED-AMR Moderators provide global coverage of AMR outbreaks/surveillance, case studies, and relevant research topics. Each ProMED-AMR alert includes subject matter expert commentary helping the reader to understand the historical context, clinical background and/or current relevance of the information.
ProMED-AMR currently has three Moderators who specialize in monitoring and reporting on AMR-related issues across the globe, including case reports, research topics, and outbreak/surveillance reporting. These Moderators include:


Ghassan Matar
Top Moderator for ProMED-MENA & ProMED-AMR
Lebanon

Salma Ferchichi
ProMED-AMR Moderator & ProMED-MENA Moderator
Tunisia

Tin Tin Myaing
ProMED-MBDS & ProMED-AMR Moderator
Thailand/Myanmar
Top Five IJID Region Research Articles Recommended for Antimicrobial Resistance Research
• Investigation and successful control of a Candida auris outbreak at a tertiary health care facility in Kenya
• The attributable mortality, length of stay, and health care costs of methicillin-resistant Staphylococcus aureus infections in Singapore
• Simultaneous clonal spread of NDM-1–producing Pseudomonas aeruginosa ST773 from Ukrainian patients in the Netherlands and Spain
• High drug-pathogen mismatch in the management of invasive carbapenem-resistant Enterobacteriaceae infections at a tertiary hospital in Nigeria
• Assessing the burden of disease of gram-negative bloodstream infections in a Brazilian hospital: A retrospective cohort study from 2015 to 2019
A Collection of Antimicrobial Resistance Research Collection and AMR Editorials from the International Journal of Infectious Diseases (IJID)
• Antimicrobial resistance research – an IJID collection of selected articles 2020-2024
• Antimicrobial resistance (AMR): ISID's global efforts to bring light to the silent pandemic (Joint Editorial of three journals)
• The battle against antimicrobial resistance is more important now than ever: time to educate, advocate and act
ESCMID World AMR Awareness Week 2024 Series
Organised by the ESCMID AMR Action Subcommittee and the International Society for Infectious Diseases (ISID)
Session 4: Global Strategy
20 November 2024, 17:00 - 18:30 CET
Introduction: Global collaboration and policymaking are essential to effectively combat AMR. This session will discuss the strategic directions from the policymakers, the specific needs of low- and lower-middle-income countries (LMICs), the potential role of vaccines in reducing AMR as well as the importance of equity within AMR policy and practice. The focus will be on actionable policies and collaborative efforts to address this global health challenge. The panelists discuss strategic directions and the opportunities for implementation of global and regional AMR Policy in the current landscape. Needs assessment in implementing AMR Policies in Low- and Middle-Income Countries will be discussed.
Chairs:
- Holger Rohde (ESCMID AMR Action Subcommittee)
- Nicholas Power
Speakers:
- Jameela Mohammed Al-Salman (Chair of the WHO Strategic Technical Advisory Group on AMR / Arabian Gulf University)
- Topic: "Global and Regional AMR Policy in a Current Landscape: Strategic Directions and The Opportunities for Implementation"
- Sujith J Chandy (Executive Director, ICARS, Denmark)
- Topic: "Assessing the needs of implementing AMR policies in LMICs"
- Connie Walyaro (ISID / Talk AB[M]R / WHO Expert Working Group on Equity and AMR)
- Topic: "Equity Perspectives of AMR Policy and Practice"
World AMR Awareness Week 2024: The role of education, advocacy, and immediate action in resource-constrained settings
A blog post written by ISID Emerging Leader Abiodun Egwuenu
Antimicrobial resistance (AMR) is not only a health issue; it is a global crisis with profound implications for societies, economies, and ecosystems. Resistant pathogens affect people everywhere, jeopardising the effectiveness of life-saving drugs and threatening lives, food security, and environmental stability. The global AMR crisis demands a multi-sectoral approach, that integrates education, advocacy, and decisive action.
The 2024 theme, “Educate. Advocate. Act now,” calls for all stakeholders—from policymakers and healthcare providers to patients and communities—to take immediate steps to address AMR.
The Global Research on Antimicrobial Resistance study, published in January 2022, reported high mortality from AMR. Out of the 4.95 million deaths globally associated with AMR in 2019, AMR was the primary cause of death in 1.27 million persons, with the condition ranking higher than HIV/AIDS or malaria in terms of mortality. Low- and middle-income countries (LMICs), especially sub-Saharan Africa and South Asia, bear the highest burden of AMR-related deaths. For example, in western sub-Saharan Africa, AMR contributed to 27.3 deaths per 100,000 people, which was significantly higher than the global average. However, these regions also lack adequate access to reliable diagnostic tools and healthcare providers prescribe antibiotics empirically, often without confirming whether an infection is bacterial, viral, or fungal. According to the World Health Organization, approximately half of bacterial infections in low- and middle-income countries (LMICs) are treated without appropriate diagnostic confirmation. Only 30%-40% of healthcare facilities in resource-constrained settings have access to essential diagnostic microbiology services, compared to over 90% in high-income countries (HICs). Antimicrobial stewardship programs are also at the infancy stage in regions with the highest burden of AMR, as 80% of the global antibiotic consumption growth is driven largely by the lack of stewardship (OECD/WHO, 2019). Access to guidelines for prescribing, tools for monitoring antibiotic use, and educating healthcare providers and the public about AMR remains suboptimal.
Limited implementation of Universal Health Coverage initiatives means that individuals often cannot afford comprehensive healthcare services. Only about 40% of the population in LMICs has some form of health insurance, compared to over 90% in most HICs (World Bank, 2021). Therefore, it is not surprising that up to 80% of antibiotic use occurs in LMIC without prescription(WHO, 2018). This financial barrier leads to self-medication with antibiotics, over-the-counter purchases without prescriptions, and incomplete antibiotic courses—all of which contribute to AMR.
The interplay between limited diagnostic access, lack of antibiotic stewardship, and restricted health insurance creates a vicious cycle that accelerates AMR in low-resource settings. Therefore, a coordinated and multi-modal response is required:
- Educate health workers and the public on the power of diagnostic access: Rapid diagnostic tools that enable clinicians to determine the type of infection – viral, bacterial, fungal etc, are required. If the infection is found to be viral, most of which are self- limiting, the clinician is no longer under pressure to prescribe antibiotics. Training healthcare workers and conducting public awareness campaigns can help patients advocate for diagnostics in the healthcare pathway.
- Advocate for establishing national and healthcare facility antimicrobial stewardship programmes: AMS initiatives promote careful management across healthcare settings, recommending narrow-spectrum agents when appropriate and optimising drug choice, dosage, and treatment duration. It is important to link them with infection prevention and control programmes and to integrate stewardship practices into healthcare systems as the standard of care. Policy reforms and accountability are necessary at all levels to include and implement stewardship as a key strategy for AMR containment.
- Act by expanding health insurance coverage for AMR interventions: Including these essential interventions, such as diagnostics, stewardship programs, and therapies in insurance programmes, increases access to responsible AMR management and reduces financial barriers to appropriate care. Expanding coverage to AMR-specific interventions supports preventive care such as vaccination and infection prevention and reduces the need for antibiotic use. Financial coverage for AMR interventions ensures timely and effective care and incentivises health systems to adopt AMR detection, prevention, and control measures.
The 2024 UNGA High-level Meeting on AMR in September has highlighted governance, access, research and development, financing, and multisectoral coordination as strategies policymakers need to enhance AMR response. Focused political leadership, dedicated resources, accountability, and shared commitment are required to sustain global AMR response gains.
References
• World Health Organization (WHO). Global Action Plan on Antimicrobial Resistance (2015).
• The Lancet Infectious Diseases. Diagnostic capacity in low-resource settings (2019).
• OECD/WHO. Antimicrobial Resistance (2019).
• World Bank. Health Insurance Coverage (2021).
• The Lancet. Antibiotic stewardship and prescribing practices (2018).
• Global Burden of Disease. AMR and Health Economics (2019)
Climate Overshoot and Antimicrobial Resistance (AMR): A One Health Challenge
A Village Membership Community blog post written by ISID Emerging Leader Abiodun Egwuenu
On November 3, 2024, One Health Day highlighted the vital connection between climate change, health, and antimicrobial resistance (AMR). Climate overshoot increases risks through agricultural pressures, ecosystem changes, and human migration, driving up antibiotic use and disease spread. Global efforts like the Paris Climate Agreement call for integrated approaches that link human, animal, and environmental health. These initiatives emphasize reducing antibiotic pollution, promoting sustainable agriculture, and building resilient health systems to tackle the intertwined challenges of climate change and AMR.
TO GAIN FULL ACCESS AND READ THIS EXCLUSIVE COMMUNITY BLOG POST, BECOME A ISID VILLAGE MEMBER TODAY

