GUIDE TO INFECTION CONTROL IN THE HEALTHCARE SETTING
THE INFECTION HAZARDS OF HUMAN CADAVERS
Authors: Peter N. Hoffman, MD; T.D. Healing, MD
Chapter Editor: Jaffar Al-Tawfiq, MD, FRCP (London), FRCP (Ireland)
The authors would like to acknowledge the contributions of the late Dr. Susan Young, who was fundamental to the structure and content of this chapter and was an author on most previous editions.
Print PDF
KEY ISSUES
Cadavers may pose hazards to those handling them. The recently dead may have been infected by a wide range of pathogens, those presenting particular risks include, tuberculosis, streptococcal infection, gastro-intestinal pathogens, the agents causing transmissible spongiform encephalopathies (e.g. Creutzfeldt-Jakob disease), hepatitis B and C, HIV infection, SARS-CoV-2, Middle East respiratory syndrome (MERS), haemorrhagic fever viruses such as Ebola, and possibly meningitis and septicaemia (especially meningococcal). None of the organisms that caused mass death in the past (e.g. plague, cholera, typhoid, tuberculosis, smallpox) is likely to survive long in burials.
KNOWN FACTS
- Most of the microorganisms that cause death do not survive for long after the host dies or are not readily transmissible in that context.
- Soft tissues remaining on a human cadaver could present an infection risk.
- Long-buried bodies reduced to skeletons are not a hazard.
- A possible hazard in old burials is anthrax, which can form resistant spores but this is unlikely.
CONTROVERSIAL ISSUES
There is a theoretical concern that smallpox may survive in buried bodies, but the risk from minimal residual virus in dry scabs is not considered to present a valid infectious testosterone enanthate for sale in usa threat. People should not be vaccinated specifically to deal with this hazard as the risk of smallpox vaccination greatly outweighs the infection risk.
SUGGESTED PRACTICE
General Considerations
Whether dealing with the recently dead or with old burials, and regardless of which infectious agents may be present, the risk of infection hazards of human cadavers can be greatly reduced by:
- Covering cuts or lesions with waterproof dressings.
- Careful cleansing of any injuries sustained during procedures.
- Good personal hygiene
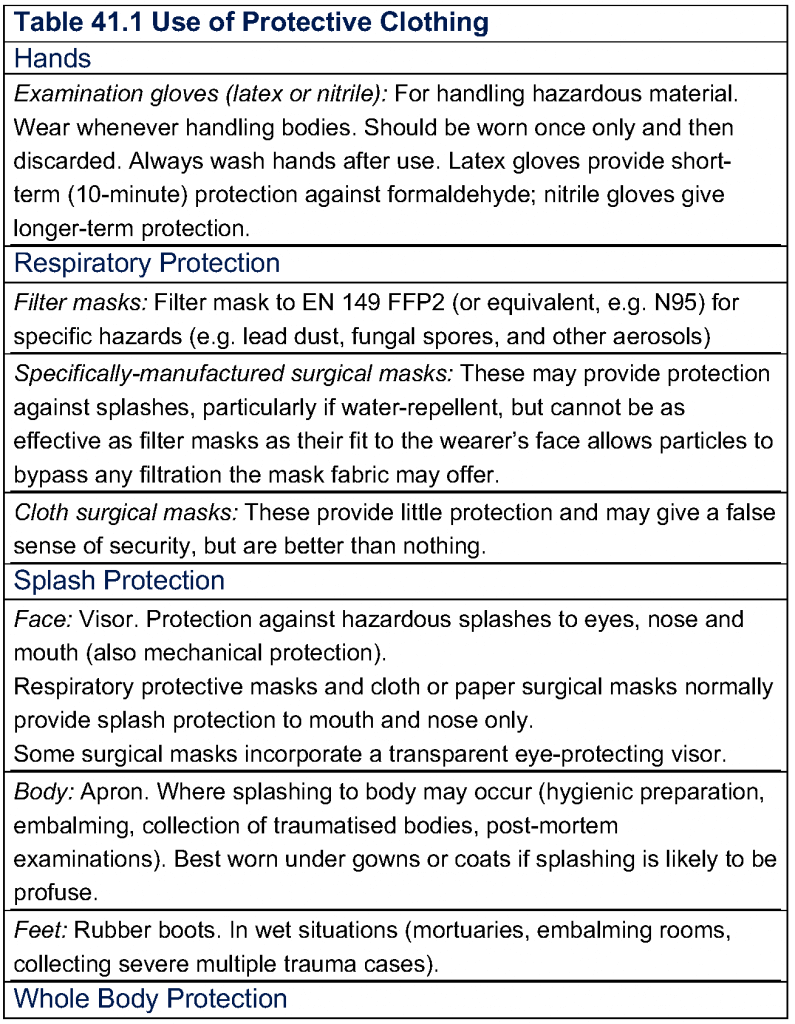
- Use of appropriate protective clothing (see Table 41.1)
Most people have little to do with the dead, although they may at some time in their lives need to deal with the human cadavers of relatives or friends during burial rituals. Some have jobs that regularly bring them into contact with human cadavers, exposing them to the risk of acquiring infections. These include doctors (especially pathologists), nurses, mortuary attendants, members of the emergency services, forensic scientists, embalmers, funeral directors and religious officials or others who routinely prepare bodies for the funeral or who perform final rites.
In most circumstances, the infected living are a much greater hazard than are the dead, even those who have died of infectious disease. Whilst a person is alive, invading pathogens can multiply and are readily transmitted; the patient is a continuing source of infection. Once the host is dead, most pathogenic microorganisms stop multiplying and die rapidly as a result of microbial competition as the body decomposes.
The Recently Dead
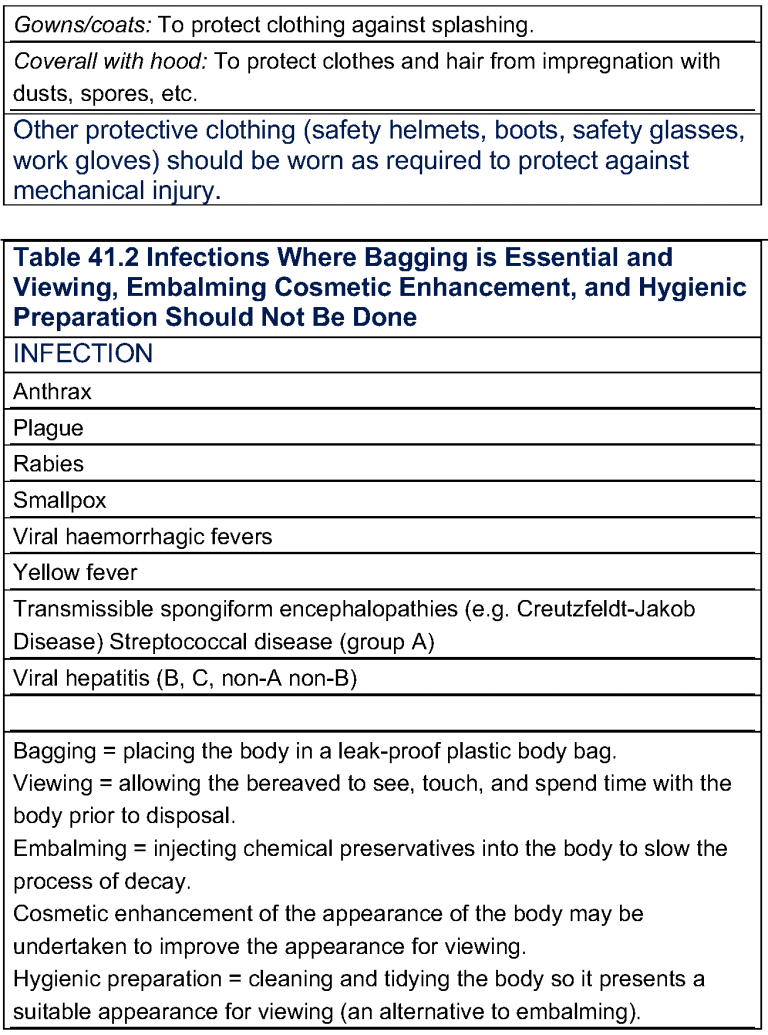
The diseases and organisms which may pose particular risks vary in different parts of the world but include tuberculosis; streptococcal infection; gastro-intestinal organisms; Creutzfeldt-Jakob disease; viral hepatitis, HIV infection, MERS, and other viral infections (particularly viral haemorrhagic fevers such as Lassa, Marburg, or Ebola); and possibly meningitis and septicaemia (especially meningococcal) (seeTable 41.2). In general, standard infection prevention practice, the use of appropriate protective clothing, will greatly reduce the risk of acquiring infection, but some additional precautions may be advisable for particular infections, for example, when dealing with infectious agents transmitted by a vector that is resident on the deceased (e.g. body lice and typhus, fleas, and plague), as these will leave the deceased and may move onto those handling the cadaver putting them at risk.
Tuberculosis
Opening human cadavers of individuals infected with tuberculosis is dangerous and workers in morbid anatomy, pathologists, mortuary technicians, and medical students have a comparatively high rate of tuberculin conversion. BCG vaccination and an annual chest X-ray are advised for such individuals. Post mortems or autopsies should be carried out with appropriate personal protective equipment and in a negative pressure or well-ventilated room.
Meningitis and Septicaemia
Meningitis can be caused by a wide range of organisms but only tuberculosis (see above) and meningococci are likely to present a risk.
Septicaemia is a common terminal event and can be caused by many different organisms (often the patient’s own flora), most of which present no hazard. Only cases of meningococcal septicaemia or of infection with group A streptococci pose a risk. Life threatening infections with the latter can result from quite trivial contact and injuries. Therefore, great care should be taken during post mortem with appropriate personal protective clothing and careful technique
Gastrointestinal Pathogens
Faecal leakage from bodies is very common. All those handling human cadavers should:
- Wear single-use gloves and impervious single-use aprons.
- Take care not to contaminate their instruments or their working environment.
- Wash their hands carefully after procedures and before eating, drinking, or smoking.
- The bodies of those who have died of diseases such as cholera or typhoid should not be buried in places where they could contaminate water sources.
Transmissible Spongiform Encephalopathies (TSEs)
These are rare conditions typically presenting as Creutzfeldt-Jakob and variant Creutzfeldt-Jakob disease. The causative agents of these diseases are highly resistant to most disinfectants and to heat. They are not inactivated reliably by chemical disinfection or conventional heat sterilisation. Only fully trained staff should undertake post mortem examinations in patients thought to be at risk of, or who are known or suspected as having, TSEs. If examination of the brain only is required, the skull should only be opened inside a large plastic bag fitted over the head and neck of the cadaver. In addition, full single-use personal protective equipment (PPE) (including coverall, apron, double gloves, full face visor, or surgical mask and eye protection) should be used. If a full post mortem is required, including the removal of viscera and spinal cord, the body should be examined in an autopsy facility that allows good infection prevention practice and is amenable to efficient environmental decontamination.
Hepatitis
- Hepatitis A is transmitted by the faecal-oral route and presents the same hazard as other gastrointestinal pathogens. A highly effective vaccine is available.
- Hepatitis B is extremely infectious and the incidence of this infection continues to increase in many countries. A highly effective vaccine is available and staff working in hospital mortuaries and embalmers should routinely receive immunisation against this infection. The bodies of those who have died of, or were known to be infected with, this virus should be handled only by those wearing full protective clothing as wounds and other sites of virus escape from bodies may not be apparent when starting a procedure.
- Hepatitis C is also highly infectious, although probably less so than hepatitis B. It is transmitted by the same routes as hepatitis B, there is no vaccine, and similar precautions to those for hepatitis B should be taken.
HIV
The routes of transmission of hepatitis B and of HIV are similar and the precautions required to prevent the transmission of the former should be adequate to prevent transmission of the latter. HIV is less infectious than hepatitis B and the risk to those handling infected human cadavers is therefore proportionately less. HIV can survive for many days post-mortem in tissues preserved under laboratory conditions. Care should be taken when handling unfixed, HIV-infected material from human cadavers, or when undertaking post-mortem examinations on those infected with HIV. Embalming the bodies of those known or suspected of being infected is not recommended.
Those infected with HIV are often infected with other organisms (such as mycobacteria), which may be more infectious (albeit less dangerous) than the HIV infection itself.
Viral Haemorrhagic Fevers (VHFs)
Viruses such as Ebola and Marburg are highly infectious and are readily transmitted by contact with infected blood, secretions, and organs. Most of the known outbreaks of these zoonotic viruses have started with individuals who acquired their infections from wildlife but have spread via healthcare facilities when staff have unknowingly become infected from the index case(s) and have subsequently spread the infection to other communities where they live and work. Great care should be exercised when dealing with those who have died of such infections and staff should be trained in the handling of cadavers in these situations. WHO advises that those who are handling the dead body of a suspected or confirmed case of VHF should wear the full set of PPE that is recommended for those treating live cases (listed below), together with heavy-duty rubber gloves.
- Double gloves (non-sterile examination gloves and outer heavy duty rubber gloves).
- A single use gown or coverall resistant to penetration by blood or body fluids.
- A waterproof apron worn over the gown or coverall. (If single use aprons are not available, heavy duty, reusable, waterproof aprons can be used if safe and thorough cleaning and disinfection with an agent likely to be active against VHFs can be achieved).
- A single-use filtering facemask giving protection equivalent to US NIOSH standard N95 or European standard FFP2.
- Eye protection (either goggles or full-face visor) in order to have the mucous membranes of the eyes, mouth, and nose completely covered by PPE and prevent virus exposure.
- Waterproof boots (e.g. rubber/ gum boots).
- Note: While those who handle the dead are unlikely to be exposed to aerosols and therefore do not need to be protected against aerosol exposure, the majority of the teams responding to the Ebola crisis in West Africa in 2014-15 found that it was best to use a single type of facial protection for all those involved with the handling of Ebola cases (despite the cost and supply implications), so as to reduce the risk of error in such a high stress situation and also to maintain morale amongst staff.
- CDC has also produced similar advisory material regarding the protection of those dealing with VHFs.
- Post-mortem examinations should not be carried out. Bodies should be bagged as soon as possible and should be buried with appropriate precautions (see below) or cremated.
SARS-CoV2 (COVID-19)
The normal route of transmission of SARS-CoV-2 is via respiratory droplets and aerosols, with the bronchial and conjunctival epithelia as the probable main points of entry. The virus can affect many organs of the body and persist for long periods in infected individuals. SARS-CoV-2 can remain viable on inanimate surfaces for up to nine days under laboratory conditions, but the importance of such contamination as a source of infection remains unclear.
At the time of writing, no SARS-CoV-2 infections in forensic pathologists or medical staff involved in mortuary or autopsy practice, that can be definitely ascribed to occupational exposure, have been reported in the literature. Seroconversion and PCR positivity have been reported in mortuary and cemetery workers, but these were most likely to have been community acquired and not occupationally acquired infections. It appears that if appropriate protective measures are followed (see below), a significant risk of occupational transmission would not be expected in these professions. However, since infectious virus has been detected in a number of cadavers for up to 38 hours and (in a single instance) has been found up to 17 days post-mortem, care needs to be taken.
With regards to preparation for burial or cremation of those who have died of SARS-CoV2 infection, the bereaved are advised to avoid rituals or practices that bring them into close contact with the deceased. If religious observance requires such contact (for example viewing, embalming, cosmetic enhancement or hygienic preparation) it should be limited to those who are wearing PPE, under the supervision of someone who is trained in the appropriate selection and use of PPE.
Guidance on the safe handling of those who have died with or from SARS-CoV-2 infection, including full autopsy procedures and the collection of specimens from cadavers, is available from several national and international sources and those dealing with such individuals are advised to follow the guidelines most relevant to their location.
Reduction of risk
- Post-mortem rooms
- Post-mortem rooms should be structured such that the risks to those working in them are minimised. Provision of adequate ventilation, lighting, running water, and good drainage is essential.
- Workers must use single-use gloves for each procedure and, after removal, wash their hands immediately.
- The environment should be cleaned with a broad-spectrum disinfectant daily.
- Instruments should either be washed in a washer-disinfector and autoclaved, or they should be cleaned and then boiled (in areas with limited resources), or immersed in a broad-range, non-corrosive disinfectant after initial cleaning. Any manual cleaning needs to be done very carefully so as to avoid the puncture of the operator's skin with sharp contaminated instruments.
- Hypochlorites (e.g. chlorine bleaches) should not be used because:
- Hypochlorite is corrosive and may damage surfaces or instruments.
- Formaldehyde is likely to be present in post-mortem rooms and the reaction between hypochlorite and formaldehyde can produce a potent carcinogen (bis-chloromethyl ether).
- Some hospital post-mortem departments bag all bodies for transfer to funeral directors. Bagging a body may be the main means by which the hospital can communicate to the funeral director that the body may present special risks, but this practice can be counter-productive in terms of safety. In countries where confidentiality precludes reference to specific infections, the type of risk involved can be identified by attaching labels advising generic precaution types (e.g. enteric, bloodborne) to the bag.
- Preparation of the dead for funerals
- Often only a simple “hygienic preparation” may be carried out either by a professional funeral worker, relatives, or religious officials. This usually involves washing the body, dressing the cadaver, tidying the hair and possibly trimming the nails and shaving. In some societies, this is an important part of the ritual of dealing with the dead (for example traditional burials in West African countries) and may involve very close contact with the human cadaver (embracing, kissing, etc.). Such rapid procedures are frequently followed in many countries, particularly the hotter ones, where burial or other disposal of the human cadaver follows death within 24 hours (either for practical or religious reasons). Under these circumstances many pathogens may still be viable but, provided there is considered to be only a low level of risk, then the use of gloves and simple protective clothing and/or good personal hygiene by anyone handling the bodies is an acceptable and effective safety measure.
- In some instances, for example where the person has died of a highly infectious disease such as Ebola or hepatitis B, even hygienic preparation is not safe (see the list of such infections in Table 41.2). Under these circumstances, the risks to those handling the human cadaver may be very high. It has been estimated that during the recent outbreak of Ebola in West Africa (2014-16) as many as 65% of those who were involved in unsafe burial practices became infected and that unsafe burial played an important role in the size and extent of the epidemic.
- Embalming may be undertaken as a means of temporary preservation by reducing microbial activity and slowing decomposition and is usually a straightforward process, but the embalming of cadavers which have been in accidents or which have been the subject of post-mortem examination is more difficult. They may be badly damaged and present particular hazards because of damaged bones, bone splinters, and (occasionally) due to sharp items, such as intravenous cannulae, left in the body. Cosmetic work on cadavers may also present hazards if the body has been damaged. There can sometimes be considerable contamination of the body with blood, faeces, and other body fluids if it is bagged, presenting an extra risk to embalmers and others involved in preparation of the body. This is another reason to avoid universal bagging of bodies by hospitals. Embalming practices such as the open drainage of the vascular system lead to excessive environmental contamination and should be avoided.
- All instruments used for embalming or for preparing bodies for the funeral should be carefully cleaned in detergent and either sterilised in an autoclave or boiled or soaked in a disinfectant. Disinfectants should be used to clean up any spills of blood or body fluid, single-use gloves being used to protect the hands from contact with the spill. Hands should always be washed after finishing a session.
- As with post-mortem rooms, hypochlorites (e.g. chlorine bleaches) should not be used (see above).
- Emergency service personnel
- The major hazard facing emergency service personnel is spilt blood and any risk can be greatly reduced by preventing contact with blood (use of gloves, face and eye protection, and protective clothing where necessary).
- Bodies that have been decaying for some time, including those that have been in water for extended periods of time, present little risk. The organisms likely to be present are their own body flora and water or other environmental organisms. The use of proper protective clothing and good personal hygiene will protect personnel handling such material.
- Bodies should always be transported to mortuary facilities in waterproof body bags or cleanable, fluid retentive (e.g. fibreglass), temporary coffins.
- Disposal of the dead
- Each society has its own methods of disposal of the deceased. These must be respected as far as possible although in a few instances (such as deaths due to highly infectious agents such as Ebola) cremation or deep burial with the cadaver in a leak-proof plastic body bag may be the only safe procedures.
- Immediately following disasters where there has been substantial loss of life, there seems to be a tradition to bury or cremate the dead as quickly as possible “to prevent the spread of disease.” In reality however, the dead bodies of disaster victims pose a minimal infectious risk to the survivors. The spectrum of disease amongst the deceased in a rapid onset disaster will be the same as that amongst the survivors. Of those deceased that had an infectious disease at the time of their death, the risk that they will disseminate it will be lower than it was during their life and those that did not have an infectious disease offer a negligible risk. The imperative of immediate disposal of the dead diverts resources from searching for and caring for the survivors at a critical time in any rescue operation. It also hampers or prevents the identification of the dead, removing part of the grieving process from their relatives, as well as prolonging their uncertainty as to the possible survival of the victims. The legal consequences of lack of identification (e.g. uncertainty of spouses about death of partners, inheritance, or welfare benefit problems) can cause long-term hardship for the deceased relatives.
- If bodies cannot immediately be identified and sufficient temporary mortuary space with refrigeration is not available, they should be buried in marked graves with at least one metre (3 feet) of earth over the cadavers (to prevent access by scavengers and pests) to allow subsequent exhumation if permitted. Careful and detailed records of such interments must be kept. Once identified, they should be dealt with following the normal religious and social practices of the affected areas as far as possible. Burial sites must be chosen so as to avoid the risks that water sources may be contaminated.
- Those handling the bodies should take basic infection control precautions: impervious gloves (single-use or disinfected after use), impervious apron or coverall, impervious footwear, and face protection if splashing is likely. Respiratory-protective masks are not necessary. The use of chloride of lime to prevent the spread of infection in these circumstances is to be avoided. It has little effect and is dangerous to those applying it. This applies equally to emergency and non-emergency situations, such as exhumations of graves and crypts.
SUGGESTED PRACTICE IN UNDER-RESOURCED SETTINGS
The practices listed above are equally applicable to under-resourced settings.
SUMMARY
Infection risks from human cadavers are of a lower level than those from living individuals who have active disease or who are carriers of infectious agents. Preventing infection of those who come into contact with those who have died of infectious disease is primarily concerned with preventing direct contact with blood and other body fluids, particularly to mucous membranes or broken skin. Such contact should be prevented by using safe procedures or, where this is not possible, the use of appropriate personal protective equipment. This should be done without compromising the dignity of the deceased and, wherever possible, not interfering excessively with the grieving processes of their relatives. In large scale natural disasters (and also in complex emergencies), the pattern of disease is generally the same in the deceased as in the survivors and the deceased present a minimal risk. The mass disposal of the remains of those who have died in such disasters should be done in such a way as to allow easy exhumation for identification purposes in the future.
REFERENCES
- Alishaq M, Jeremijenko A, Nafady-Hego H et al. SARS-CoV-2 infection in mortuary and cemetery workers. International Journal of Infectious Diseases VOLUME 105, P621-625, APRIL 01, 2021. https://www.ijidonline.com/article/S1201-9712(21)00229-0/fulltext
- UK Department of Health, Health and Safety Executive (HSE). Advisory Committee on Dangerous Pathogens. Management of Hazard Group 4 Viral Haemorrhagic Fevers and Similar Human Infectious Diseases of High Consequence. 2015; available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/534002/Management_of_VHF_A.pdf
- Ball J, Desselberger U, Whitwell H. Long-Lasting Viability of HIV After Patient's Death. Lancet 1991; 338(8758):63.
- Collection and Submission of Postmortem Specimens from Deceased Persons with Confirmed or Suspected COVID-19. Updated Dec. 2, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-postmortem-specimens.html
- Guidance on Personal Protective Equipment (PPE) to be Used by Healthcare Workers During Management of Patients with Confirmed Ebola or Persons Under Investigation (PUIs) for Ebola Who are Clinically Unstable or Have Bleeding, Vomiting, or Diarrhea in US Hospitals, Including Procedures for Donning and Doffing PPE. (August 2015); available at https://www.cdc.gov/vhf/ebola/healthcare-us/ppe/guidance.html
- Department of Health England. National Resource for Infection Control (NRIC). Guidance on Prevention of CJD and vCJD by Advisory Committee on Dangerous Pathogens' Transmissible Spongiform Encephalopathy (ACDP TSE) Risk Management Subgroup. Annex H: After death. 2012; available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/209766/Annex_H_-_After_death.pdf
- Gamble MR. Hazard: Formaldehyde and Hypochlorites. Laboratory Anim 1977; 11(1):61.
- Hawkey PM, Pedler SJ, Southall PJ. Streptococcus pyogenes: a Forgotten Occupational Hazard in the Mortuary. Br Med J. 1980; 281(6247):1058.
- Health and Safety Executive (HSE). Managing infection risks when handling the deceased. Guidance for the mortuary, post-mortem room and funeral premises, and during exhumation. July 2018. https://www.hse.gov.uk/pubns/books/hsg283.htm
- Heinrich F, Meißner K, Langenwalder F et al. Postmortem Stability of SARS-CoV-2 in Nasopharyngeal Mucosa. Emerg Infect Dis. 2021;27(1):329-331. https://doi.org/10.3201/eid2701.203112
- COVID-19: General Guidance for the Management of the Dead. 16 June 2020. https://www.icrc.org/en/publication/covid-19-general-guidance-management-dead
- Morris SI. Tuberculosis as an Occupational Hazard During Medical Training. Am Rev Tuberc. 1946; 54:140–58.
- Morgan O. Infectious Disease Risks from Dead Bodies Following Natural Disasters. Rev Panam Salud Publica. 2004; 15(5):307–12.
- Newsom SWB, Rowlands C, Matthews J, Elliott CJ. Aerosols in the Mortuary. J Clin Pathol 1983; 36(2):127–32.
- Pan American Health Organization. Management of Dead Bodies in Disaster Situations: a Field Manual for First Responders. (2nd (revised) Edition). Washington, DC: PAHO, 2016; available at http://www.paho.org/disasters/index.php?option=com_content&view=article&id=666:management-of-dead-bodies-in-disaster-situations&Itemid=924
- Plenzig S, Bojkova D, Held H. et al. Infectivity of deceased COVID-19 patients. Int J Legal Med 135, 2055–2060 (2021). https://doi.org/10.1007/s00414-021-02546-7
- Public Health England. Guidance for care of the deceased with suspected or confirmed coronavirus (COVID-19) (Updated 15 December 2021). https://www.gov.uk/government/publications/covid-19-guidance-for-care-of-the-deceased/guidance-for-care-of-the-deceased-with-suspected-or-confirmed-coronavirus-covid-19
- Public Health England. (Deceased Management Advisory Group). COVID-19: guidance for managing a funeral in England during the coronavirus pandemic. (2020).(Updated April 2021) http://www.dmag2020.org/important-updated-guidance-covid-19-guidance-for-managing-a-funeral-during-the-coronavirus-pandemic-4/
- Royal College of Pathologists. (Osborn M, Lucas S, Stewart R, et al ). Autopsy practice relating to possible cases of COVID-19 (2019-nCov, novel coronavirus from China 2019/2020). https://www.rcpath.org/uploads/assets/d5e28baf-5789-4b0f-acecfe370eee6223/447e37d0-29dd-4994-a11fe27b93de0905/Briefing-on-COVID-19-autopsy-Feb-2020.pdf
- Smith GS. Tuberculosis as a Necropsy Room Hazard. J Clin Pathol 1953; 6(2):132–4.
- Tiffany A, Dalziel BD, Kagume Njenge H, et al. Estimating the Number of Secondary Ebola Cases from an Unsafe Burial and Risk Factors for Transmission of the West Africa Ebola Epidemic. PLoS Negl Trop Dis. 2017; 11(6):e0005491. doi: 10.1371/journal.pntd.0005491; available at https://doi.org/10.1371/journal.pntd.0005491.
- de Ville de Goyet C. Stop Propagating Disaster Myths. Lancet. 2000; 356(9231):762–4.
- West DJ. The Risk of Hepatitis B Infection Among Health Professionals in the United States: a Review. Am J Med Sci. 1984; 287(2):26–33.
- Wolff HL, Croon JAB. The Survival of Smallpox Virus (Variola Minor) in Natural Circumstances. Bull World Health Organ. 1968; 38(3):492–3.
- World Health Organization. (2020). Infection prevention and control for the safe management of a dead body in the context of COVID-19: interim guidance. 4 September 2020. World Health Organization. https://www.who.int/publications/i/item/infection-prevention-and-control-for-the-safe-management-of-a-dead-body-in-the-context-of-covid-19-interim-guidance
- WHO. Interim Infection Prevention and Control Guidance for Care of Patients with Suspected or Confirmed Filovirus Hemorrhagic Fever in Health-Care Settings, with Focus on Ebola. (August 2014); available at http://www.who.int/csr/resources/publications/ebola/filovirus_infection_control/en/
