GUIDE TO INFECTION CONTROL IN THE HEALTHCARE SETTING
HEALTHCARE WORKERS AS A SOURCE OF TRANSMISSION
Author: Margreet C. Vos, MD, PhD
Chapter Editor: Ziad A. Memish, MD, FRCPC, FACP
Print PDF
KEY ISSUES
Within the hospital, healthcare workers (HCWs) are often exposed to infections. Any transmissible disease can occur in the hospital setting and may affect HCWs. HCWs are not only at risk of acquiring infections but also of being a source of infection to patients. Therefore, both the patient and the HCW need to be protected from contracting or transmitting hospital-acquired infections by using recommended infection control measures.
KNOWN FACTS
- The infection control objectives of a hospital should be planned by the infection control committee and occupational health services. The focus of the committee and services must be personal hygiene, monitoring of carriage of specific microorganisms, monitoring of infectious disease outbreaks and exposures and, after identifying infection risks, institution of preventive measures.
- Prevention of infectious diseases in HCWs serves three purposes: the health of the healthcare worker, the prevention of work restrictions, and the reduction of hospital-acquired infections. The latter is discussed in this chapter.
- Education is an important factor for improving compliance with guidelines and prevention measures. All HCWs need to know about the risk of infection and the route of transmission of pathogens. Hand hygiene and standard precautions are the foundation for preventing transmission of infectious diseases to patients.
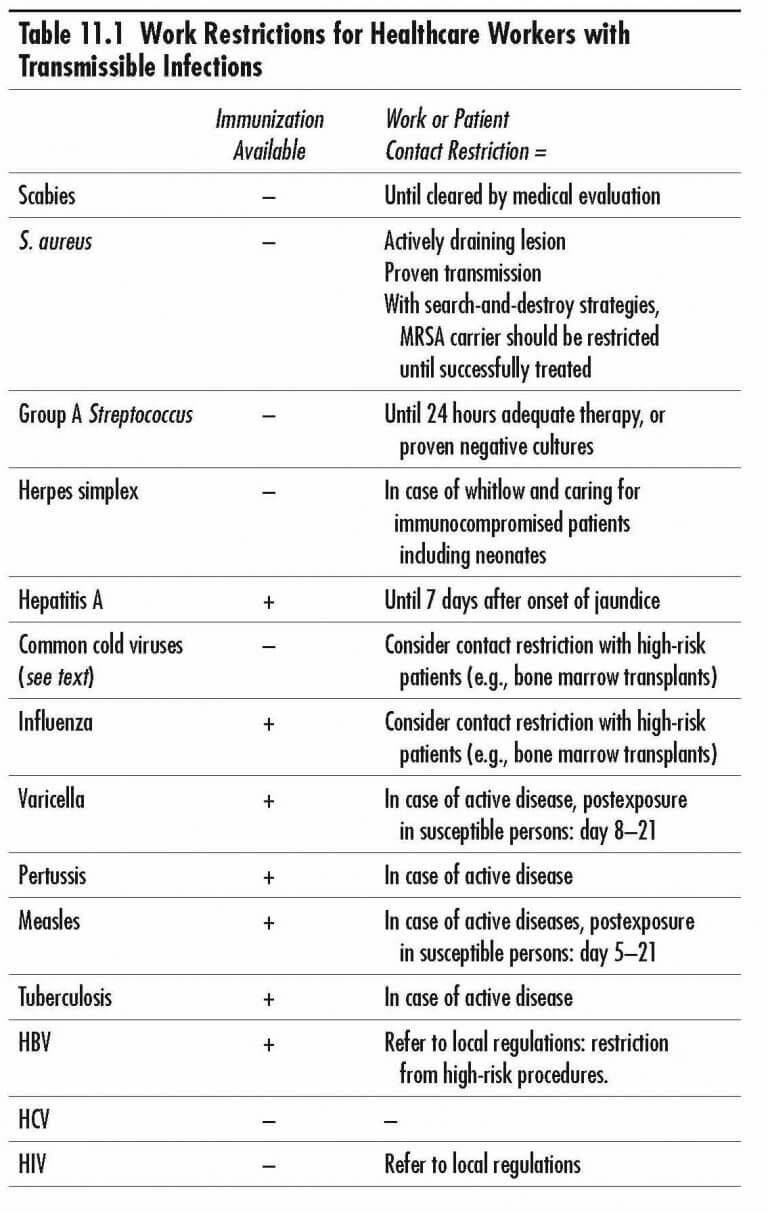
- Immunization should be used to protect HCWs from specific infectious agents. Preventing infections in HCWs will also prevent transmission of infections from HCWs to patients. Prompt evaluation of and institution of appropriate control measures for patients with signs and symptoms of transmissible infectious diseases will reduce the risk of hospital-acquired diseases.
- In deciding the type of infection control procedures needed, one must consider the HCW’s job, risk of exposure, and the suspected infectious pathogen.
Infectious Diseases Transmitted by Healthcare Workers
A short overview of some of the most important infectious diseases transmitted by HCWs is presented below.
SUGGESTED PRACTICE
General Principles
In a recent review, 152 hospital-acquired infection outbreaks with a HCW as a source were identified. These outbreaks were mainly associated with surgery, neonatology, and gynecology departments. The most frequently encountered pathogens were hepatitis B virus, Staphylococcus aureus, and Streptococcus pyogenes.
In general, the most important infection prevention measure is adequate hand hygiene. Hand disinfection as defined by the WHO guidelines specifies 5 moments of hand hygiene. In short this comprises;
- before touching a patient
- before clean/aspect procedure
- after body fluid exposure risk
- after touching a patient
- after touching patient surroundings
Skin Infections
Scabies
Scabies is transmitted by direct contact. In case of Norwegian (crusted) scabies, transmission is also through fomites, such as bed linens, floors, walls, furniture, clothes, and the air. Symptoms of intense pruritus can develop 2 to 6 weeks after initial infestation. To prevent infection and to prevent a hospital outbreak, a HCW with skin exposure should receive prophylactic therapy, and to prevent re-infestation, the household contacts should be treated too. In case of scabies crustosa, contact persons should be identified and should receive prophylactic treatment. Contact patients are those who shared the room or were otherwise direct or indirect exposed to skin scales. Contact health care workers are those having cared for the patient without taking precautions measures. Immunocompromised patients have a high chance of developing scabies crustosa, which is harder to recognize compared to “local” scabies and is more infectious.
Staphylococcus aureus
About one-third of the population are persistent nasal carriers of S. aureus(SA), one-third are intermittent carriers, and one-third are unaffected. Other sites of colonization are the throat, perineum, skin, axilla, or hair. People with dermal lesions, such as eczema, are more likely to be carriers. Carriers may spread SA to patients, especially patients with wounds, intravascular catheters, and other indwelling catheters. Dissemination of SA is by direct or indirect contact or, less commonly, by skin scales. Healthcare workers with active lesions caused by SA such as boils (even on an occult body area) or other skin lesions are more likely to transmit infection to others than nasal carriers. HCWs who are carriers of methicillin-resistant S. aureus(MRSA) are a high risk to patients, by transmitting MRSA from their skin, hands, or nose to wounds or mucosal surfaces. MRSA seems to spread more easily than methicillin-sensitive S. aureus (MSSA), probably due to selection during antibiotic use and probably not due to the presence of other virulence mechanisms in mecA positive microorganisms.
During periods of high incidence of staphylococcal disease or epidemics of MRSA, identifying carriers by culturing patients and HCWs is useful. Carriers can be treated with 2% mupirocin ointment and disinfective soap washing. The optimal strategy for identifying and decolonizing HCWs who carry MRSA is unknown. In some countries, HCWs with MRSA carriage are not allowed to perform patient related activities. This, to stop the transmission circle. This underscores the importance of preventing acquiring MRSA during work by implementing general preventive measures.
Group A Streptococcus
Group A Streptococcus(GAS) is a well-known pathogen of the skin and pharynx. Other reservoirs include the rectum and the female genital tract. Major modes of transmission are direct contact and large droplets. An increased incidence of wound infections by GAS should be investigated. Particular focus should be placed on carriage by HCWs. Healthcare workers with overt infection due to GAS should be restricted from work until 24 hours after adequate therapy has been given or until cultures are proven to be negative. Overall, the risk of transmission of GAS from HCW to patients is considered low.
Herpes simplex
Herpes simplex type 1 can be transmitted from HCWs to patients through primary or recurrent lesions. Most infections are orofacial and transmitted by direct contact. Saliva also can be infectious. Because the main route of transmission is by contaminated hands after direct contact with the lesion, handwashing, and disinfection before and after patient contact are the most important methods for preventing transmission to patients. Herpes simplex lesions of the fingers (herpetic whitlow) are an occupational disease of HCWs due to direct exposure to contaminated fluid such as vaginal secretions or skin lesions. Healthcare workers with herpetic whitlow must use gloves to prevent the spread of the herpes virus to patients. When caring for patients at risk of severe infection, such as preterm neonates, patients with severe malnutrition, severely burned, or immunocompromised patients, restriction of work of HCWs with herpes infections should be considered.
Enteric Diseases
Acute Diarrhea
Transmission of most microorganisms causing diarrhea in HCWs is by direct or indirect contact. Careful handwashing, especially after visiting the bathroom, is the most important measure for preventing transmission of these pathogens. Until symptoms are resolved, healthcare workers with acute infectious diarrhea should not care for patients. Even after resolution of the acute disease, HCWs may still carry enteric pathogens.
HCWs can be asymptomatic carriers of Salmonella spp or Campylobacterspp during the convalescent period or a protracted period thereafter. Testing for carriage may be unreliable and is therefore usually limited to food handlers, who are more likely to transmit disease to others. Careful hand washing after using the bathroom and before patient contact will prevent the transmission of enteric pathogens from most carriers. Antibiotic treatment is rarely indicated.
In case of norovirus, HCWs can be an important link in hospital outbreaks: infected HCWs may be asymptomatic upon arrival at work, get ill suddenly and consequently spread the virus by vomiting. On the other hand, they can be infected by patients. Patients should be isolated and HCWs should be sent home in the event that they manifest active disease. The advent of PCR testing makes the diagnosis of norovirus more feasible. During an outbreak of norovirus, hand hygiene with soap and water is preferable to alcohol based hand sanitizers.
Hepatitis A
Hepatitis A occurs rather infrequently as a hospital acquired infection. Prevention of transmission is through maintaining personal hygiene, especially through hand washing.
Respiratory Diseases
Common Cold
The common cold in adults is caused by the influenza virus, parainfluenza virus, adenovirus, rhinovirus, or respiratory syncytial virus. HCWs are important sources of these viruses to patients. In general, to prevent hospital-acquired transmission from HCWs to patients, infected HCWs should wash or disinfect their hands carefully before patient contact. The use of masks is optional but may be helpful in preventing transmission due to large droplets upon close contact. Routine use of gloves has no additional benefit; even if gloves are used, hands should be disinfected or washed after gloves are removed. In most people, viral upper respiratory infections are self-limiting. However, in immunocompromised patients, such as recipients of bone marrow transplants, these infections may progress to severe lower respiratory tract diseases with very high mortality rates. Infection control strategies include identifying, cohorting, and isolating of infected patients and limiting contact of symptomatic HCWs and visitors with high-risk patients. Work restrictions for symptomatic HCWs may be considered, especially when working with immunocompromised patients.
Influenza
Influenza epidemics are well known in hospitals. Transmission occurs from HCWs to other HCWs and patients, and from patients to HCWs and other patients. Hospital infection control committees should implement an influenza vaccination program each year, several weeks before the influenza season. There is evidence that vaccination is associated with decreases in mortality, the number of febrile respiratory illness days, and HCW absenteeism. During periods of influenza activity, personnel with acute febrile respiratory infections should not provide care to high-risk patients. The incubation period is 1 day before onset of symptoms and the period of communicability is from 1 day before until 7 days after onset of symptoms. Additionally, prophylactic antiviral agents may be used. Hospitals should have written guidelines for avian and pandemic influenza.
Middle East Respiratory Coronavirus (MERS-CoV)
MERS-CoV is a relatively new coronavirus discovered in September 2012, and still rare causes of respiratory infections outside the Arabian Peninsula. MERS-CoV can cause serious respiratory infections with high mortality. At least 750 of 2144 laboratory-confirmed cases had died from this infection (data as of March 2018). However, MERS-CoV can also present as an asymptomatic or a mild disease. Outbreaks among HCWs of MERS-CoV have been described which highlight the importance of continued vigilance and detailed systematic screening of exposed HCWs. It is recommended to test all the HCWs who have been in close contact to a case of MERS-CoV. In the WHO recommendations for surveillance, published in June 2015, close contact is defined as “health-care associated exposure, including providing direct care for MERS‐CoV patients, working with HCWs infected with MERS‐CoV, visiting patients or staying in the same close environment (sharing classroom, housing, and travel in any conveyance) of a MERS‐CoV patient. Ideally, those who are exposed and asymptomatic should be screened and returned to work only if they have 2 negative results 24 hours apart. In case of extreme shortage of personnel the asymptomatic HCW can be allowed to work with non-immunocompromised patients as long as he/she wears mask if within 1 meter (3 feet) of patients or staff and use good hand hygiene practices. The HCW will be actively monitored for signs and symptoms and should be tested weekly until negative and repeat testing in 24 hours for confirmation of negativity. HCWs should be excluded from work if they develop MERS-CoV–like symptoms. Recently in case of MERS-CoV, it has been reported that asymptomatic HCWs were able to transmit the virus to other HCWs, despite being asymptomatic.
Pertussis
Vaccination of adults with whole-cell (Wc P) Bordetella pertussisvaccine is not recommended because of local and systemic reactions. The acellular vaccine (aP) has been used for attempted control of hospital pertussis outbreaks but clinical effectiveness has not been proven. Active disease in HCWs should trigger a search for potentially exposed patients. Infection prevention measures should be taken. These include giving prophylactic antibiotic treatment to exposed neonates with low or negative IgG levels as these patients are at high risk for developing severe pertussis.
Varicella zoster
Varicella zoster virus causes varicella or chickenpox in childhood. After years, due to reactivation, the virus can manifest as skin lesions (zoster or shingles), which may be widely disseminated in immunocompromised patients. Those lesions can be infectious to others through direct contact and cause varicella in susceptible persons.
Varicella is one of the most common hospital-acquired diseases among HCWs. It is a highly contagious disease and exposure to the virus is common in the healthcare setting. Most persons with a clear history of chickenpox in childhood are probably immune. Persons with a negative history can be immune but should be tested. Susceptible HCWs may acquire infection after exposure to infectious patients. Non-immune HCWs exposed to varicella should be excluded from work from days 8 to 21 after contact, to ensure that infection has not occurred. If the HCW develops disease, he/she should be excluded from work until all lesions are dry and crusty. Since such a policy regarding work restriction is very expensive, vaccination of all susceptible workers should be done. A live-attenuated varicella vaccine was licensed for use in several, but not in all countries. Vaccination provides approximately 70% protection against infection and 95% protection against severe disease for 7 to 10 years after vaccination. Vaccination of HCWs is proven to be cost-effective.
Measles
Measles is transmitted by the airborne route. The same strategy as has been recommended for varicella-susceptible HCWs can be followed for susceptible HCWs exposed to measles. Prompt identification of HCWs and patients with rash and fever will help prevent further spread of this virus. HCWs need to have documented measles immunity prior to working in healthcare facilities.
Tuberculosis
The infection control committee should indicate high-risk wards, were HCWs are routinely screened on tuberculosis. After conversion of the Mantoux tuberculin test, or positive other newly developed screening tests (IGRA/interferon gamma release assay), prophylactic treatment is indicated to prevent open tuberculosis which is contagious for patients. Furthermore, all HCWs reporting symptoms suggestive of tuberculosis should have a medical examination and a chest radiograph. Suggestive symptoms are cough for more than 3 weeks, persistent fever, and weight loss. After identifying an HCW suffering from open tuberculosis, a prompt evaluation of all contacts must be instituted. Stringent measures regarding work restrictions are necessary. Healthcare workers should be receiving effective treatment and have negative sputum smears before returning to work. Bacille Calmette-Guérin (BCG) vaccination should be considered for all tuberculin skin test negative HCWs, unless previously vaccinated, in countries where tuberculosis is endemic or in hospitals where exposure to infectious TB cases is likely.
Bloodborne Pathogens
The management of HCWs infected with bloodborne pathogens has been reviewed by the AIDS/TB committee of the Society for Healthcare Epidemiology of America (SHEA). Recently, an updated CDC recommendation for the management of hepatitis B virus-infected healthcare providers and students was published. In general, prevention of infection is based on appropriate infection control procedures to avoid blood contact from patient to HCW and from HCW to patient. The major emphasis is on applying blood precautions, practicing hand washing, minimizing contact with blood or blood-contaminated excretions, and handling all blood as potentially infectious. Education concerning bloodborne pathogens for all healthcare workers is recommended, not just those who are already infected.
Hepatitis B
Immunization with the hepatitis B virus (HBV) vaccine is the most important measure to prevent infection of the HCW by HBV. Each hospital must develop an immunization strategy. Healthcare workers with active HBV or those who are carriers of HBV are at risk for transmitting the virus to others. The risk of transmission of HBV is higher than that of the hepatitis C virus or the human immunodeficiency virus, as is reflected in 38 outbreaks of HBV by HCW-to-patient transmission in the past 22 years.
Vaginal hysterectomy, major pelvic surgery, and cardiac surgery are associated with HBV transmission despite the use of proper infection control measures. With these surgeries, the chances of needle-stick injuries are presumably greater. Before increased use of infection control interventions, the risk of HBV transmission was also associated with dental procedures. The presence of high numbers of HBV-DNA copies in source HCW is almost always the case. Another route of transmission can be by hepatitis B positive HCWs with exudative dermatitis on body areas that may come in contact with patients.
Restricting HCWs from practice of gynecologic or (cardiac) surgery or performing dental procedures should be not be judged by the presence of a HBV infection only. The risk of transmission should be carefully established and monitored. The risk of transmission to patients, despite appropriate use of infection control measures, depends on the procedures performed and the levels of HBV-DNA. Treatment of the HBV infection can possibly decrease the number of copies of HBV-DNA below critical levels. Defined critical levels of the HBV-DNA vary between countries. For HBV positive HCWs who perform exposure-prone procedures, an expert panel should provide oversight of the HCWs practice and risk of transmission.
Human Immunodeficiency Virus (HIV) and Hepatitis C Virus (HCV)
The risk of transmission of HIV is probably 100 times lower than hepatitis B, with that of HCV being somewhere between HIV and HBV. Healthcare workers known to be infected with HIV or HCV are strongly recommended to follow universal precautions as recommended in their hospital to minimize the risk of infection to others. Using double gloves for procedures is recommended. HIV- and HCV-infected HCWs should not be prohibited from patient care activities solely on the basis of their infection. Healthcare workers need not be screened routinely for HIV or HCV infection, except in cases of significant exposure of a patient to the blood or body fluid of an HCW.
AIDS
Healthcare workers infected with HIV can be infected with HIV-associated pathogens. In turn, these pathogens can be transmissible to patients. Examples are Mycobacterium tuberculosis, varicella zoster, and measles by aerogenic spread and Salmonella spp, Cryptosporidium spp, and all other enteric pathogens via fecal-oral exposure. For prevention of transmission, see the relevant part of this chapter.
Vaccine-Preventable Diseases
Healthcare workers may be exposed to vaccine-preventable diseases and then, after contracting the disease, be infectious to patients. It is recommended that HCWs be vaccinated or have demonstrated immunity to certain vaccine-preventable diseases. The infection control committee of each hospital has to develop policies requiring proof of immunity or, if needed, offer vaccination. Herd immunity of the hospital community is not reliable and unvaccinated HCWs are a potential risk to patients. For HCWs, the following diseases are vaccine-preventable and can be transmitted to patients during healthcare work; varicella, measles, pertussis, influenza A, hepatitis B, and hepatitis A.
REFERENCES
- Bell DM, Shapiro CN, Ciesielski CA, Chamberland ME. Preventing Bloodborne Pathogen Transmission from Healthcare Workers to Patients: The CDC Perspective. Surg Clin North Am 1995; 75:1189–203.
- Bolyard EA, Tablan OC, Williams WW, et al. Guideline for Infection Control in Healthcare Personnel, 1998. Infect Control Hosp Epidemiol 1998; 19(6):407–63.
- CDC: Immunization of Healthcare Workers: Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the Hospital Infections Control Practices Advisory Committee (HICPAC). MMWR. 1997; 46(RR-18):1–42.
- Chandler RE, Lee LE, Townes JM, Taplitz RA. Transmission of Group A StreptococcusLimited to Healthcare Workers with Exposure in the Operating Room. Infect Control Hosp Epidemiol 2006; 27(11):1159–63.
- Danzmann L, Gastmeier P, Schwab F, Vonberg RP. Healthcare Workers Causing Large Nosocomial Outbreaks: a Systematic Review. BMC Infect Dis. 2013; 13:98. doi: 10.1186/1471-2334-13-98.
- Kuehnert MJ, Cardo DM, Infections Associated with Healthcare Personnel: Vaccine-Preventable Diseases and Bloodborne Pathogens. Curr Infect Dis Rep 2000; 2(6):475–83.
- Ofner-Agostini M, Gravel D, McDonald LC, et al. A Cluster of Cases of Severe Acute Respiratory Syndrome Among Toronto Healthcare Workers After Implementation of Infection Control Precautions: A Case Series. Infect Control Hosp Epidemiol. 2006; 27(5):473–8.
- Shefer L, Dales L, Nelson M, et al. Use and Safety of Acellular Pertussis Vaccine Among Adult Hospital Staff During an Outbreak of Pertussis. J Infect Dis. 1995; 171(4):1053-6.
- WHO Guidelines on Hand Hygiene in Health Care. 2009; available at http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf.
- Updated CDC Recommendations for the Management of Hepatitis B Virus–Infected Healthcare Providers and Students. MMWR Recomm Rep. 2012; 61(RR-3):1–12.
- Interim Infection Prevention and Control Recommendations for Hospitalized Patients with Middle East Respiratory Syndrome Coronavirus (MERS-CoV). 2015; available at https://www.cdc.gov/coronavirus/mers/infection-prevention-control.html.
- Command and Control Center Ministry of Health Kingdom of Saudi Arabia Scientific Advisory Board. Infection Prevention and Control Guidelines for the Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Infection (4th Edition). 2017; available at http://www.moh.gov.sa/endepts/Infection/Documents/Guidelines-for-MERS-CoV.PDF.
- Alfaraj SH, Al-Tawfiq JA, Altuwaijri TA, et al. Middle East Respiratory Syndrome Coronavirus Transmission among Health Care Workers: Implication for Infection Control. Am J Infect Control. 2018; 46(2):165–8. doi: 10.1016/j.ajic.2017.08.010.
